Stroke Information

WHAT IS A STROKE?
A stroke occurs when blood supply to the brain is disrupted. This will typically lead to weakness or numbness on one side of the face, arm or leg.
- There are two kinds of strokes:
- Ischemic Stroke: Caused by a blockage in an artery in the brain due to a clot or narrowing in the artery
- Hemorrhagic Stroke: Caused by sudden leakage or bursting of an artery
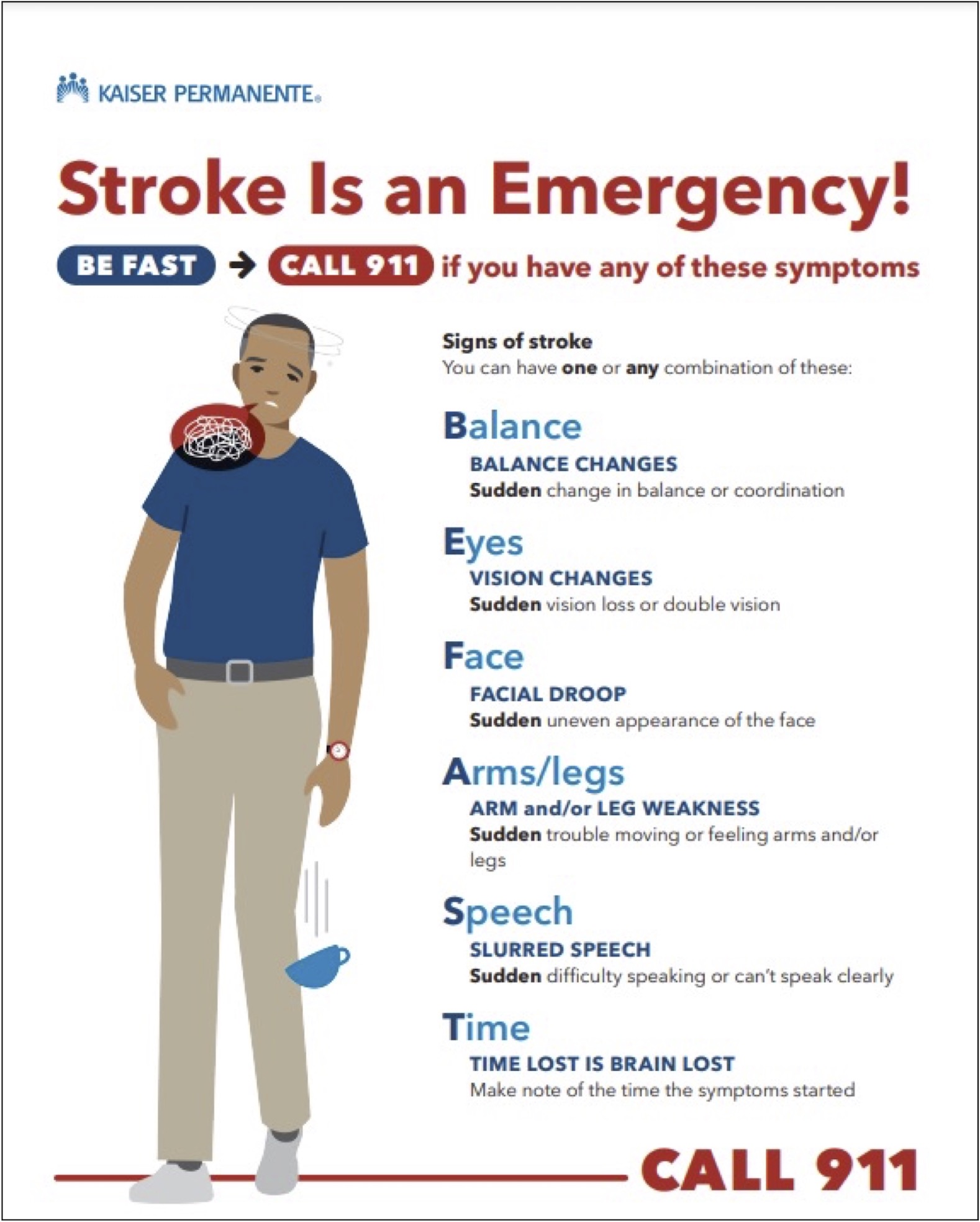
SYMPTOMS OF A STROKE
WHAT IS A TRANSIENT ISCHEMIC ATTACK (TIA)?
- This is a brief disruption in blood supply to the brain.
- Symptoms of a TIA are similar to those that can be seen in a stroke (please see stroke symptoms)
- Luckily, because blood supply is quickly restored, symptoms of this potential stroke may resolve. Transient ischemic attacks can typically come before an actual stroke may happen.
- Patients who experience a transient ischemic attack should call 9-1-1 and seek immediate emergency medical attention.
WHAT ARE THE LONG-LASTING EFFECTS OF A STROKE?
- When brain cells suffer a stroke, it is considered a permanent injury. As such, a stroke can leave serious, long-lasting effects. If a stroke is untreated, permanent paralysis, speech and swallowing problems, visual disturbances and inability to wake up may persist.
- It is very important to seek immediate medical attention by dialing 9-1-1 if you or someone near you is suffering a stroke.
- In cases of hemorrhagic stroke, immediate medical attention can reduce the expansion of the bleed.
- In cases of ischemic stroke, immediate medical attention may include treatment with a clot busting medication (IV-tPA) and possibly the removal of the clot (Thrombectomy)
TYPE OF STROKES TREATED AT KAISER PERMANENTE LOS ANGELES MEDICAL CENTER
- Ischemic stroke
- Hemorrhagic stroke
- Intra-parenchymal hemorrhage
- Subdural/epidural hematoma
- Subarachnoid hemorrhage
CONDITIONS AND TREATMENTS:
Ischemic Stroke
Ischemic stroke is caused by the disruption of blood flow to the brain, due to a blockage or narrowing of an artery in the brain.
Symptoms
- As with any stroke, symptoms can include sudden onset weakness or numbness on one side of the body, sudden onset speech or swallowing problems, trouble walking, or vision problems.
Causes
- Carotid Artery Disease
- Intracranial Artery Stenosis
- Small Vessel Ischemic Infarct
- Atrial Fibrillation (Afib)
- Hypercoagulable State
Preventive Treatment
- Treatments depend on the underlying cause of ischemic stroke, however, modification of Risk Factors will decrease the risk of stroke.
- Modification of Risk Factors
- Lifestyle changes that are known to reduce ischemic stroke and TIA include:
- Keeping your blood pressure under control..
- Managing diabetes.
- Stopping tobacco use.
- Lowering high cholesterol.
- Managing afib and other heart conditions.
- Managing carotid stenosis and other arterial (heart) diseases with medication or surgery, if necessary.
- Limiting alcohol consumption and avoiding drug use.
- Getting regular physical activity and maintaining a healthy weight.
- Lifestyle changes that are known to reduce ischemic stroke and TIA include:
- Carotid Artery Disease
- The carotid arteries are the two main arteries that supply the front, left, and right parts of the brain. When plaque builds up on the artery walls, the arteries become narrowed and the amount of blood flow to the brain is reduced. This happens due to either severe narrowing of the artery, or a piece of clot rupturing from the plaque, blocking an artery further downstream.
- Patients who suffer from carotid artery disease with a corresponding TIA or ischemic stroke should be evaluated for possible surgery (Carotid Endarterectomy or Carotid Artery Stenting) to help lower their risk of further strokes.
- Intracranial artery stenosis
- Strokes can also occur if there is a direct narrowing of the arteries in the brain. Typically, maximum medical therapy is recommended with aspirin, clopidogrel and a cholesterol medication. Controlling modifiable risk factors is also important. Routine intervention with the placement of stents and angiogplasty is not recommended as first-line therapy; although can be considered in particular cases.
- Small Vessel Ischemic Infarct
- Chronic high blood pressure and diabetes can cause a type of stroke called a small vessel ischemic infarct. This type of stroke occurs when the smaller, deeper, root-like vessels in the brain build up with micro clots and eventually close off. Although these types of strokes are small, they tend to cause significant symptoms and often affect your strength and sensation. A neurologist would identify a small vessel ischemic infarct after reviewing its location and your risk factors.
- Being on an antiplatelet (such as aspirin, Aggrenox or clopidogrel) and cholesterol-lowering medications can help prevent strokes. Ultimately, addressing modifiable risk factors will be key.
- Atrial Fibrillation
- Atrial fibrillation is an abnormality in the rhythm of the heart. When blood tends to stagnate in the heart due to abnormal rhythms such as atrial fibrillation, there is an increased risk of developing clots that travel up to the brain. This can cause an ischemic stroke.
- Depending on your risk factors, your doctor can help you decide whether or not you would benefit from being on an anticoagulant to prevent further strokes. If you have atrial fibrillation, you can view your risk of strokes annually here: (CHADS2 VASC calculator)
- Hypercoagulable states Underlying genetic factors can cause a person to have “thickened blood” or hypercoagulable states. Certain hypercoagulable states may need to be anticoagulated. While there are many causes, you should speak to your doctor about which testing is appropriate for you if you have had a stroke.
Acute Treatment in Ischemic Stroke – IV-tPA
- When a patient suffers an acute ischemic stroke, they can potentially receive a clot-busting medication named IV-tPA if they seek care within 4.5 hours of the start of the symptoms.
- IV-tPA has about a 40% chance of helping improve a patient’s outcome from a stroke.
- A multidisciplinary team will evaluate the patient during a code stroke to see if the patient is a good candidate to receive IV-tPA.
- As noted, time is a very important component of stroke care. If you or someone near you is suffering a stroke, call 9-1-1 immediately.
Acute Treatment in Ischemic Stroke – Thrombectomy
- A thrombectomy is the physical removal of a clot. A person may be a candidate for a thrombectomy if they:
- have suffered an acute ischemic stroke.
- have a visible clot blocking a major blood vessel in the brain.
- Thrombectomy is not an open surgery. It is a procedure that involves accessing the brain arteries through the arteries near the groin.
- As noted, time is a very important component of stroke care. If you or someone near you is suffering a stroke, call 9-1-1 immediately.
- Hemorrhagic stroke is a rupture or tearing of a blood vessel in the brain, causing bleeding in the brain. Hemorrhagic strokes are categorized based on the location of the bleed.
- Epidural hemorrhage
- Subdural hemorrhage
- Subarachnoid hemorrhage
- Intra-parenchymal hemorrhage
- Epidural and Subdural Hemorrhage
- Epidural and subdural hemorrhages are bleeds on the surface of the brain which are typically caused by trauma or accumulate over time. These types of bleeds are typically managed by a neurosurgeon.
- If the bleed is causing significant pressure and shifting of the brain, surgery may be necessary.
- Subarachnoid Hemorrhage
- A subarachnoid hemorrhage is a bleed that is typically located on the outside surface of the brain, usually at the base.
- The predominant symptom for this type of stroke is a headache. Other signs and symptoms are the same as those for a standard stroke.
- A subarachnoid hemorrhage is typically caused by an aneurysm that may have ruptured.
- Treatment involves
- Securing the aneurysm by either clipping or coiling, to prevent further bleeding.
- Reversing any medications which may have contributed to extra thinned blood.
- Extensive ICU management of medical conditions and Neurosurgical capabilities to manage complications of:
- Rebleeding.
- Further strokes that may develop in the brain.
- Seizures.
- Increased intracranial pressure.
- Concurrent heart injury.
- Intra-parenchymal hemorrhage
- Intra-parenchymal hemorrhages occur when there is blood within the brain tissue itself. Intraparenchymal hemorrhages have many different causes.
- Treatment:
- Typically consists of dealing with the underlying cause.
- Includes controlling blood pressure and reversing any excessive thinness of blood due to medications.
- Causes of Intra-Parenchymal Hemorrhages
- Hypertensive Hemorrhage
- This is the most common cause of an intra-parenchymal hemorrhage. Typical locations of bleed in the deeper parts of the brain along with elevated blood pressures are consistent with hypertensive hemorrhages. The best way to treat and prevent hypertensive hemorrhage is by keeping blood pressure under control.
- Amyloid Angiopathy
- Protein deposits in the small vessels in the brain cause the vessels to be brittle. This leads to increased risks of bleeding. While there is no clear preventative therapy at this time, keeping blood pressure under control and avoiding anticoagulation is likely beneficial.
- Arterial Vascular Malformation
- Abnormal connections between the artery and the veins can lead to rupture and bleeding in the brain. These malformations can be evaluated with blood vessel imaging. Treatment typically involves endovascular treatment, performed by a neurointerventionalist.
- Hemorrhagic Conversion of Ischemic Stroke
- Sometimes an ischemic stroke can convert and bleed. Any type of injury in the brain leads to fragile tissue, which can sometimes bleed. Treatment again involves controlling your blood pressure and holding any antiplatelet or anticoagulants until your doctor says it is safe to resume.
- Coagulopathy
- Being on blood thinners or having an inherent genetic condition can cause bleeding in the brain. Immediate treatment involves reversing the thinness of the blood.
- As with any of these causes of hemorrhage, medical treatment with blood pressure control and addressing the underlying cause of the bleed is the mainstay of treatment.
- Hypertensive Hemorrhage